Managed care pharmacy often sounds like a secretive corner of the profession — something that happens behind the scenes, far from the retail counters and hospital floors most are familiar with. But in reality, managed care pharmacy is about ensuring patients receive the right medications, at the right cost, and with the best possible outcomes. It encompasses a wide range of career paths that touch nearly every part of the healthcare system.
Pharmacy Benefit Management
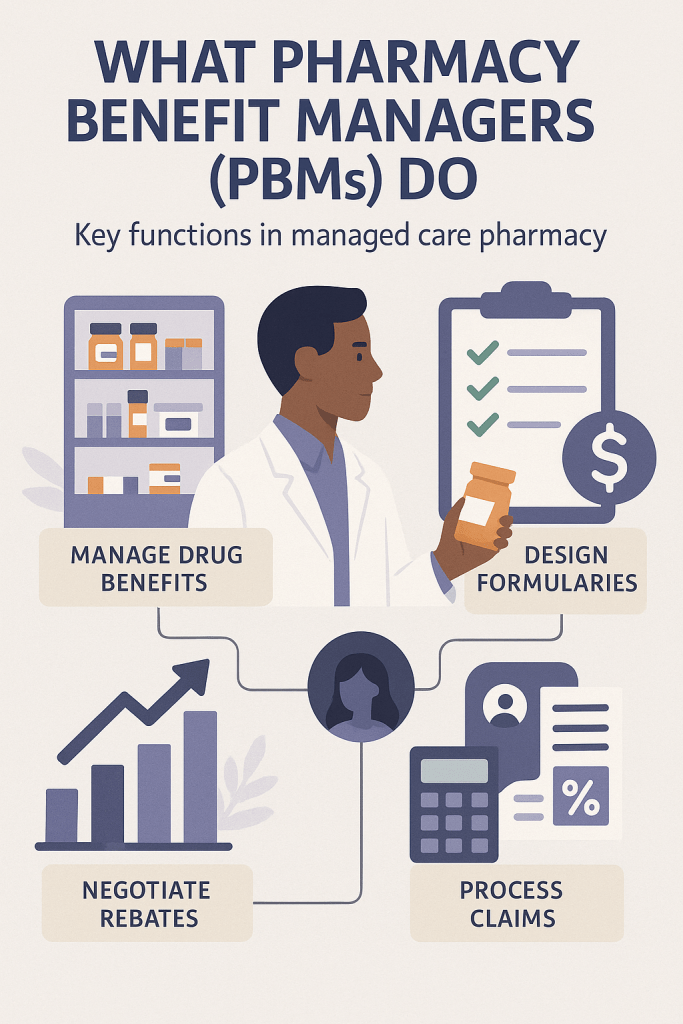
While Managed Care Organizations (MCOs) manage the full range of healthcare services — including medical, pharmacy, and other benefits — Pharmacy Benefit Managers (PBMs) focus specifically on administering the pharmacy benefit. PBMs are typically contracted by MCOs, employers, and government programs to help control drug costs, support appropriate medication use, and streamline pharmacy-related operations. They act as the middle layer between drug manufacturers, pharmacies, and health plans. Their key responsibilities include creating and managing drug formularies, negotiating rebates and discounts, and implementing tools like prior authorizations, step therapy, and quantity limits to ensure safe, cost-effective prescribing. PBMs also manage pharmacy networks and determine members’ out-of-pocket costs at the pharmacy.
Beyond clinical strategies, PBMs handle several operational functions that health plans may either manage in-house or outsource. These include processing pharmacy claims, operating call centers to support member questions, and overseeing programs that promote medication adherence and quality of care. While often working behind the scenes, PBMs play a major role in shaping the prescription drug experience for patients, providers, and payers alike.
Formulary and Utilization Management
Another core area of managed care pharmacy is formulary and utilization management — where clinical judgment meets strategic decision-making. While PBMs often lead formulary development, managed care pharmacists play a central role in evaluating medications and designing policies that guide how and when drugs are used. These strategies are essential to balancing patient care with affordability.

Formulary management involves building and maintaining a list of covered medications based on clinical effectiveness, safety, and cost. Pharmacists collaborate closely with physicians and other experts through Pharmacy & Therapeutics (P&T) Committees to review clinical trial data, real-world evidence, and therapeutic alternatives. Utilization management (UM) complements this work by ensuring that medications are used appropriately and efficiently. Common UM tools include prior authorization (requiring clinical criteria before a drug is approved), step therapy (trying a preferred drug first), and quantity limits (restricting supply to promote safe use). Together, formulary and UM strategies support high-quality care, avoid unnecessary costs, and help protect patients from potentially inappropriate therapies.
Clinical Programs
Beyond formulary and utilization management, clinical programs represent another impactful area of managed care pharmacy. These programs are designed to improve medication use, promote better health outcomes, and reduce avoidable healthcare costs. Managed care pharmacists help design and oversee these initiatives by identifying gaps in care, supporting member adherence, and addressing complex medication needs — especially for patients with chronic or high-risk conditions.
Examples of clinical programs include medication therapy management (MTM), adherence monitoring, opioid safety programs, care transition support, and disease-specific interventions (such as for diabetes, asthma, or hypertension). Pharmacists use claims data, lab results, and patient profiles to identify members who may benefit from extra support, then collaborate with providers, case managers, and members directly. These programs reflect the growing role of pharmacists not just as medication experts, but as population health partners within managed care.
Quality
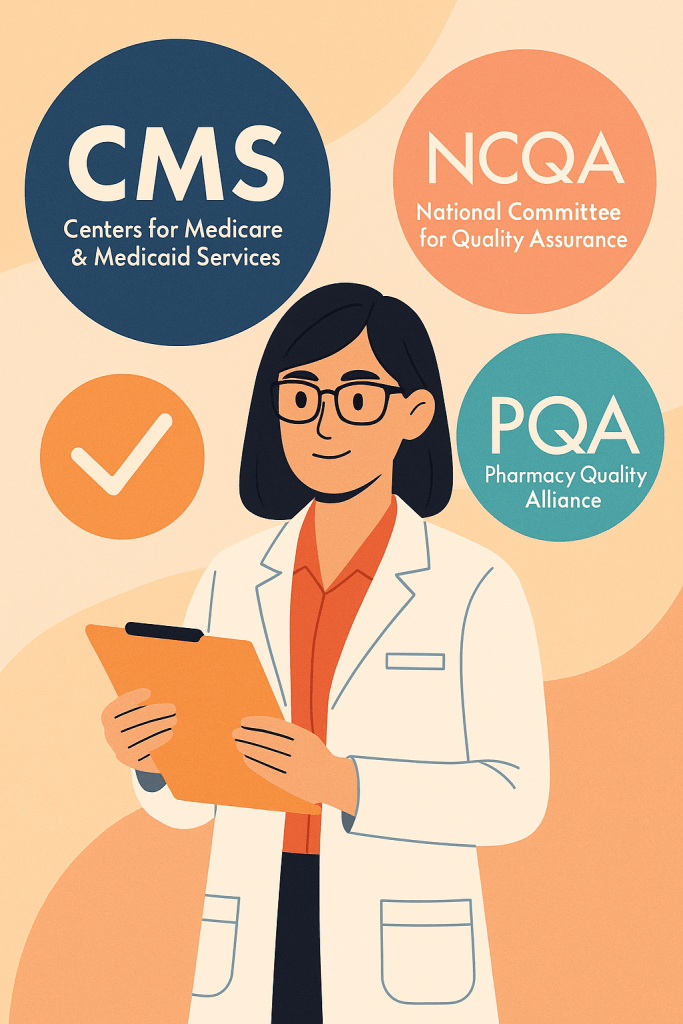
Quality is a foundational pillar in managed care pharmacy, tying together formulary decisions, clinical programs, and patient outcomes. Health plans are held accountable for delivering high-value care, and pharmacists play a key role in meeting quality benchmarks set by organizations such as the Centers for Medicare & Medicaid Services (CMS), the National Committee for Quality Assurance (NCQA), and the Pharmacy Quality Alliance (PQA). These benchmarks influence plan ratings, reimbursement, and ultimately, member trust.
Managed care pharmacists support quality initiatives by monitoring medication adherence, reducing inappropriate prescribing, and improving outcomes in chronic conditions such as diabetes, hypertension, and high cholesterol. They analyze performance metrics, develop strategies to close care gaps, and collaborate with providers to promote evidence-based practices. Whether enhancing star ratings or improving member experience, pharmacists help ensure medication-related care contributes meaningfully to a plan’s overall quality goals.
Conclusion
Together, these areas — formulary and utilization management, clinical programs, and quality initiatives — form the foundation of managed care pharmacy. While each serves a distinct function, they are deeply interconnected, working in concert to ensure patients receive safe, effective, and affordable medication therapy. Managed care pharmacists play a central role in this ecosystem: applying clinical expertise, leveraging data to guide decisions, and collaborating across teams to support both individual member needs and broader population health goals. By integrating these strategies, managed care pharmacy doesn’t just manage medications — it drives meaningful improvements in healthcare delivery.
